Up to 75% of cow diseases occur within the first month post-calving — making this phase critical for long-term health and productivity. While transition management traditionally focused on metabolic disorders such as ketosis and hypocalcemia, new research invites us to take a more holistic and preventive approach, placing inflammation as a cornerstone of transition disorders.

Global Marketing Manager Ruminant Feed Additives
Lallemand Animal Nutrition
INFLAMMATION: THE MISSING LINK
Beyond metabolic issues like ketosis and hypocalcemia, inflammation is emerging as a central factor in transition cow health.
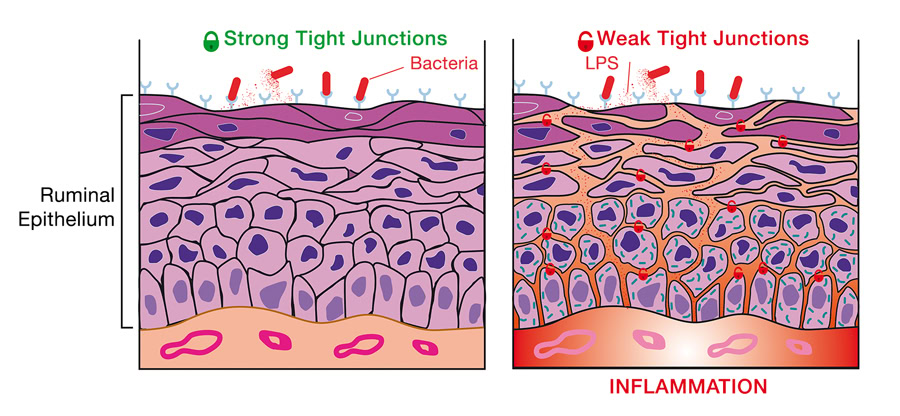
A shift to lactating rations (higher energy and protein) during the transition period changes the microbiota balance in the rumen: There is a decrease in fibrolytic microbiota (bacteria and fungi) and an increase in rapidly fermentable carbohydrate degraders. This switch decreases rumen pH and can lead to a higher risk for subacute ruminal acidosis (SARA) that damages the rumen wall epithelium.
On the other hand, tight junctions, which are a key component of the rumen epithelial barrier, are also disrupted, leading to increased permeability of the rumen epithelium. A compromised epithelial barrier, or leaky epithelium, of either the rumen or lower gut, results in bacteria translocation leading to excessive immune activation and inflammation (Figure 1).
From calving stress to oxidative stress, other factors converge to activate the immune system and divert energy from milk production.
First of all, the increased metabolic demand, along with the demands of the developing calf, can lead to an elevated production of reactive oxygen species (ROS) as byproducts of metabolism. A disruption in the balance between ROS and antioxidants is the definition of oxidative stress, which can also contribute to inflammation and immune dysregulation.

Moreover, stress, common around calving, activates the hypothalamic pituitary-adrenal axis, leading to the release of corticotropin-releasing factor (CRF), which can disrupt the intestinal barrier and contribute to systemic inflammation.
The increased energy demand of the immune system causes the animal to shift its metabolic priorities, negatively affecting growth, reproduction and productivity.
![]() THE TRUE COST OF INFLAMMATION
THE TRUE COST OF INFLAMMATION
Inflammation redirects energy from milk synthesis to immune defense — costing up to 26 kg of milk every day!
During immune activation associated with increased intestinal barrier permeability, metabolism normally dedicated to milk synthesis, that normally requires 25-30% of basal metabolism in a healthy animal, is redirected towards the immune system. The immune system requires a great deal of energy. Once under pressure, this requirement increases, which consumes nutrients.
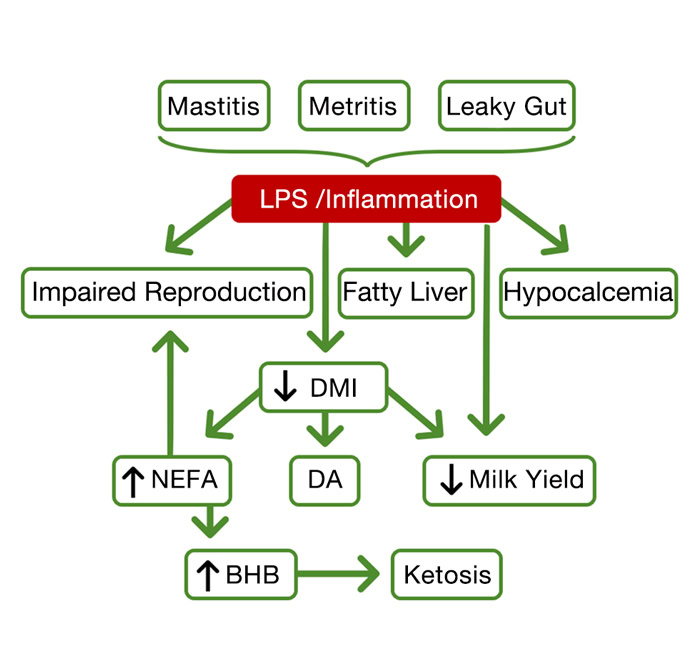
The cow will find energy sources including glucose as precursor of lactose, which are intermediaries as the cow mobilizes fat stores as a source of energy. If the inflammation becomes pathological, it reduces feed intake and may result in metabolic syndromes such as hypocalcemia.
The use of glucose by the immune system and the reduction in feed intake are responsible for the increase in NEFA (non-esterified fatty acids) and ketones, explaining a decline in overall health, production, and reproduction outcomes.
Recent studies show that the energy to fight against inflammation (modeled by LPS-induced infection) costs the equivalent of 2 kg of sugar every day and approximately 26 kg of milk loss.
(adapted from Horst E.A. et al., 2021)
POST-PARTUM DISORDERS: INFLAMMATION’S RIPPLE EFFECT
Inflammation can also cause post-partum disorders in dairy cows, such as ketosis, milk fever (hypocalcemia), reproductive tract infections such as retained fetal membranes, metritis, and endometritis. All of these can negatively impact the cow’s health, fertility, and milk production.
For example, ketosis, which occurs when the cow mobilizes excessive fat for energy, leads to an accumulation of ketone bodies, resulting in a decrease in milk quality and fertility. Research shows that inflammation during the transition period negatively impacts cow reproductive performance as it decreases ovarian activity (Figure 2).
EXPERT TIPS TO REDUCE INFLAMMATION
As Professor Mike Steele, a specialist in physiology and metabolism of dairy calves and transition cows, at the University of Guelph, explains during an interview: “We want to do everything we can to minimize inflammation in early lactation. Inflammation comes from stress. It can be gastrointestinal disorders or abrupt dietary changes. But it can also be an important change in the cow’s environment, or a really rough calving or mastitis.”
When asked how a dairy farmer can decrease inflammation, Steele shares his own approach, focusing on nutrition and beyond: “Decreasing inflammation can come from many different areas. Personally, I focus on the gastrointestinal tract. We look at ways of adapting the diet from a dry cow diet to an early lactation diet to minimize leaky gut.” However, he adds that, while nutrition is important, we also should focus on overall management practices and the animal environment, since “inflammation can come from everywhere”.
DIGESTIVE WELFARE STARTS WITH MICROBIOTA MANAGEMENT
Supporting optimal microbiota balance is essential to prevent leaky epitheliums as gut barrier disruption leads to increased permeability and inflammation. Reducing leaky rumen epithelium by maintaining a balanced microflora can be achieved by supplementing a probiotic live yeast, the rumen-specific yeast strain S. cerevisiae CNCM I-1077 (Levucell SC, Lallemand Animal Nutrition). Research has shown that S. cerevisiae CNCM I-1077 limits inflammation at the epithelium level (strengthens rumen post-calving), boosting DMI post-calving and milk production. When supplemented before calving, the live yeast strain helps the rumen wall better prepare for the stress encountered around calving by improving rumen wall integrity (tight junctions) and resistance to rumen wall inflammation through its effects on cytokines.
In a trial performed during early lactation (IRTA, Spain, 2019), Levucell SC fed cows were shown to produce 6 liters of extra milk, partly explained by a higher DMI of 2.5 kg/head/day. This higher DMI was equivalent to a higher non-fiber carbohydrate (NFC) intake in the Levucell SC group of 1.21 kg, equivalent to an extra 20%, corresponding to a higher energy supply.
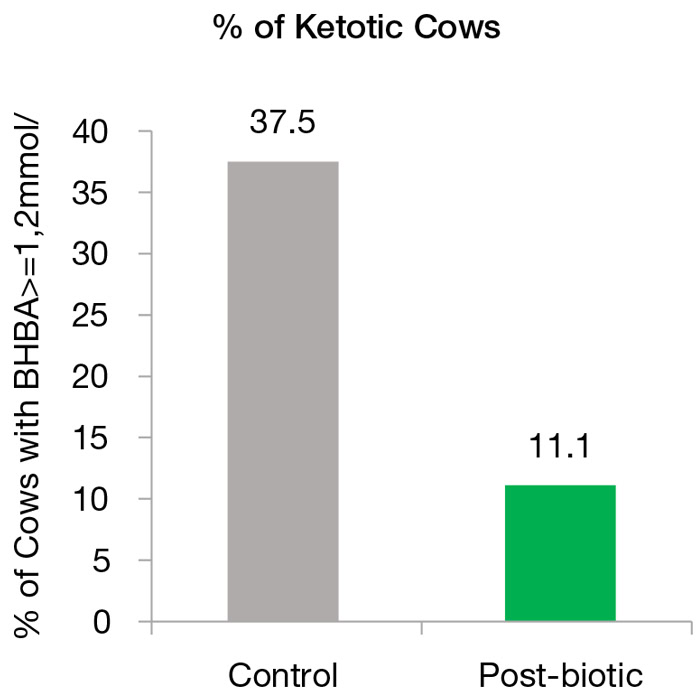
In another commercial trial with Holstein transition cows, Poland (2015), the same rumen-specific live yeast combined with specific yeast product from Lallemand, reduced the number of ketotic cows by 26.4% compared to the control group (Figure 3).
CONCLUSION
Leaky epitheliums are the central cause of inflammation and immune activation during the transition period; with consequences on health and productivity. Nutritional strategies that support gut integrity and reduce inflammation are essential for a smooth and successful transition period.
Among other animal management practices not detailed in this article, pro and postbiotic feed additives that can help maintain balanced rumen microbiota and epithelial integrity during the transition period can support cow health and high performance under such challenging conditions, yielding high economic outcomes.
References
1. Boylen, K. 2022, April 6. The common denominator: leaky gut syndrome. Progressive Dairy | Ag Proud. https://www.agproud.com/articles/28372-the-common-denominator-leaky-gut-syndrome
2. Horst, E., Kvidera, S., & Baumgard, L. 2021. Invited review: The influence of immune activation on transition cow health and performance—A critical evaluation of traditional dogmas. Journal of Dairy Science, 104(8), 8380–8410. https://doi.org/10.3168/jds.2021-20330
About Marie-Valentine Glica
An agronomist Marie-Valentine Glica has been working for Lallemand Animal Nutrition for 5 years as global ruminant marketing manager. Glica is in charge of marketing and communication for the feed additives range (trial valorization, on-farm services and training tools development). She has previous experience in technico-marketing in healthcare for large and young ruminants.